Back pain is an extremely common complaint – it's estimated that over 60% of people suffer from it at some time in their lives. And it's one of the main reasons for taking time off work.
Causes of back pain
Back pain can strike anyone at any age, although figures show you are most vulnerable if you are between 45 and 59.
But the seriousness of the condition varies. If the pain lasts for less than three months, you have what is called acute back pain. If your problem goes on for longer, you are suffering from chronic back pain.
But the seriousness of the condition varies. If the pain lasts for less than three months, you have what is called acute back pain. If your problem goes on for longer, you are suffering from chronic back pain.
If you experience acute back pain, it's quite likely to have a simple cause – this is the case with 95% of all cases of acute back pain. Most people who suffer from this sort of back pain are adults up to 55 years old who are otherwise healthy. The pain is short-lived, and has quite a simple physical cause – though it may well be due to strain over time, rather than the result of overdoing it just once.
The pain is based in the lower back, and maybe also in the buttocks and thighs. It will come and go at different times, and depending on what you are doing.
You may get simple back pain if:
The pain is based in the lower back, and maybe also in the buttocks and thighs. It will come and go at different times, and depending on what you are doing.
You may get simple back pain if:
- you have a poor posture
- you don't get enough exercise
- you stand or bend down for long periods
- your chair doesn't provide enough back support
- your mattress doesn't provide enough back support
- you lift, carry, push or pull loads that are simply too heavy for you, or you go about these tasks in the wrong way
- you trip or fall over
Back pain can be a symptom of more serious problems
In a relatively small number of cases, back pain may have a more serious underlying cause. This includes abnormality of the spine, an infection or collapse of the vertebrae, fibromyalgia (a condition that affects the muscles), tuberculosis or cancer.
These kinds of problems are more likely to be the case if your back pain starts gradually, gets worse over time, and seems unrelated to how active you are. You'll also be very likely to have other symptoms including, for example, incontinence or general tiredness or lethargy. You're also more at risk if you have had certain other conditions, especially tuberculosis or cancer, in the past.
Most attacks of simple back pain last only a few days and get better on their own. But you should see a doctor straightaway if you have any of the following symptoms as well as your back pain:
These kinds of problems are more likely to be the case if your back pain starts gradually, gets worse over time, and seems unrelated to how active you are. You'll also be very likely to have other symptoms including, for example, incontinence or general tiredness or lethargy. You're also more at risk if you have had certain other conditions, especially tuberculosis or cancer, in the past.
Most attacks of simple back pain last only a few days and get better on their own. But you should see a doctor straightaway if you have any of the following symptoms as well as your back pain:
- fever
- redness or swelling on your back
- pain down your legs and below your knees
- numbness or weakness in one or both of your legs
- loss of bladder or bowel control
- your pain lasts longer than a week
- it's the result of an injury, a fall or blow to your back
Diagnosis of back pain
In most cases, your doctor will only need to discuss your symptoms and examine you. Your doctor is likely to refer you for more tests only if your pain lasts longer than six weeks, or if he or she suspects there is some underlying cause of the pain.
These tests might include:
These tests might include:
- X-rays
- CT (computerised tomography) scans
Treatment of back pain
Activity
Research shows that bed rest does not help simple back pain - it's much better for you to return to normal physical activity as soon as possible. Staying active may hurt more at first, but it helps your back to heal quickly, and reduces the risk of the problem occurring again.
If you really can't cope, and feel you have no option but to take to your bed, try to limit it to two or three days before you are up and about again.
Painkillers
Paracetemol or ibuprofen are usually enough to relieve simple back pain. Muscle relaxants such as diazepam may help if you have muscle spasms, but do not take them for more than a week. And try applying a hot water bottle or an ice pack to the painful area - these can both offer some relief.
Manipulation and exercises
Osteopathy and chiropractic - treatments involving manipulation of your spine - may provide short-term relief for simple back pain within the first six weeks. However, you should only consult an osteopath or chiropractor who is a registered practitioner. Back exercises and physiotherapy may be helpful if your pain lasts longer.
Complementary approaches
The Alexander Technique may help improve your posture. Acupuncture can help with the pain. And, because back pain can sometimes be a sign of emotional problems, counselling may also be helpful.
Surgery
If you have a chronic back problem that is not helped by manipulation, exercises or medication, surgery may solve or help the problem. If your pain is caused by, say, a damaged disc, this could be surgically removed.
Research shows that bed rest does not help simple back pain - it's much better for you to return to normal physical activity as soon as possible. Staying active may hurt more at first, but it helps your back to heal quickly, and reduces the risk of the problem occurring again.
If you really can't cope, and feel you have no option but to take to your bed, try to limit it to two or three days before you are up and about again.
Painkillers
Paracetemol or ibuprofen are usually enough to relieve simple back pain. Muscle relaxants such as diazepam may help if you have muscle spasms, but do not take them for more than a week. And try applying a hot water bottle or an ice pack to the painful area - these can both offer some relief.
Manipulation and exercises
Osteopathy and chiropractic - treatments involving manipulation of your spine - may provide short-term relief for simple back pain within the first six weeks. However, you should only consult an osteopath or chiropractor who is a registered practitioner. Back exercises and physiotherapy may be helpful if your pain lasts longer.
Complementary approaches
The Alexander Technique may help improve your posture. Acupuncture can help with the pain. And, because back pain can sometimes be a sign of emotional problems, counselling may also be helpful.
Surgery
If you have a chronic back problem that is not helped by manipulation, exercises or medication, surgery may solve or help the problem. If your pain is caused by, say, a damaged disc, this could be surgically removed.
Managing back pain
Good back care can greatly reduce your risk of back pain. To look after your back, make sure you:
- take regular exercise
- use a chair with a backrest, and sit with your feet flat on the floor or on a foot rest
- sleep on a firm mattress
- Lift only a manageable weight, or ask for help.
- When lifting, bend your knees, keep your back straight and your feet apart.
- Do not lift and twist at the same time.
- Lift and carry objects close to your body.
- Bend your knees, not your back, when you put things down
How your back works
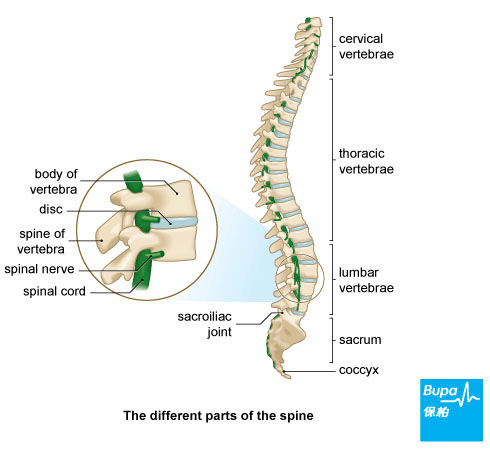
Your spine is made up of many small bones called vertebrae. These are separated by discs, which allow the spine to bend. This structure of vertebrae and discs is supported along its length by muscles and ligaments. Your spinal cord threads through the centre of each vertebra, carrying nerves from your brain to the rest of your body.
Disclaimer
This information was published by Bupa Group's Health Content Team and has been reviewed by appropriate medical or clinical professionals. To the best of their knowledge the information is current and based on reputable sources of medical evidence, however Bupa (Asia) Limited makes no representation or warranty as to the completeness or accuracy of the Content.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.










