Bowel cancer, also known as colorectal cancer, is the name for any cancer of your large bowel and rectum (back passage). Very rarely, cancers can occur in your small bowel.
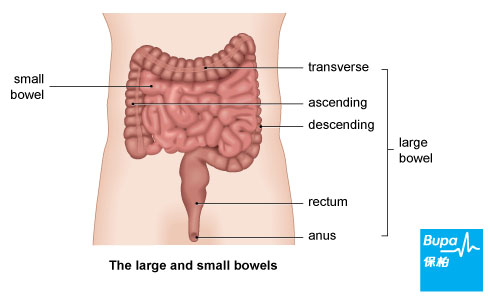
Your large bowel (also called your colon) is the last section of your digestive system. Food passes through your small bowel (the longer, thinner part of your bowel) where nutrients are absorbed. Food waste then travels through your large bowel, where it becomes more solid faeces.
Your large bowel has three sections: the ascending; transverse; and descending colon. Your rectum, at the end of your large bowel, is where faeces collects before passing through your anus as a bowel movement.
Usually, large bowel cancers develop from small, non-cancerous (benign) growths of tissue called polyps that can extend from the lining of your bowel wall. Sometimes polyps can become cancerous (malignant) over time. If the cancer isn't treated, it can grow through the wall of your bowel and spread to other parts of your body.
Your large bowel (also called your colon) is the last section of your digestive system. Food passes through your small bowel (the longer, thinner part of your bowel) where nutrients are absorbed. Food waste then travels through your large bowel, where it becomes more solid faeces.
Your large bowel has three sections: the ascending; transverse; and descending colon. Your rectum, at the end of your large bowel, is where faeces collects before passing through your anus as a bowel movement.
Usually, large bowel cancers develop from small, non-cancerous (benign) growths of tissue called polyps that can extend from the lining of your bowel wall. Sometimes polyps can become cancerous (malignant) over time. If the cancer isn't treated, it can grow through the wall of your bowel and spread to other parts of your body.
Causes of bowel cancer
The causes of bowel cancer aren't fully understood at present. One of the main factors is increasing age.
Your risk of bowel cancer also increases if you have:a family history of bowel cancerone of two inherited bowel conditions that increase your risk - familial adenomatous polyposis (FAP) or hereditary non-polyposis colorectal cancer (HNPCC), also known as Lynch syndromea long-term bowel condition, such as Crohn's disease or ulcerative colitisa diet that is low in fibre and fruit and vegetables and high in red and processed meatsan inactive lifestyle, or are obesediabetes
Your risk of bowel cancer also increases if you have:a family history of bowel cancerone of two inherited bowel conditions that increase your risk - familial adenomatous polyposis (FAP) or hereditary non-polyposis colorectal cancer (HNPCC), also known as Lynch syndromea long-term bowel condition, such as Crohn's disease or ulcerative colitisa diet that is low in fibre and fruit and vegetables and high in red and processed meatsan inactive lifestyle, or are obesediabetes
Causes of bowel cancer
The causes of bowel cancer aren't fully understood at present. One of the main factors is increasing age.
Your risk of bowel cancer also increases if you have:a family history of bowel cancerone of two inherited bowel conditions that increase your risk - familial adenomatous polyposis (FAP) or hereditary non-polyposis colorectal cancer (HNPCC), also known as Lynch syndromea long-term bowel condition, such as Crohn's disease or ulcerative colitisa diet that is low in fibre and fruit and vegetables and high in red and processed meatsan inactive lifestyle, or are obesediabetes
Your risk of bowel cancer also increases if you have:a family history of bowel cancerone of two inherited bowel conditions that increase your risk - familial adenomatous polyposis (FAP) or hereditary non-polyposis colorectal cancer (HNPCC), also known as Lynch syndromea long-term bowel condition, such as Crohn's disease or ulcerative colitisa diet that is low in fibre and fruit and vegetables and high in red and processed meatsan inactive lifestyle, or are obesediabetes
Symptoms of bowel cancer
Bowel cancer is often painless in the early stages, but there are symptoms, including:
- blood in your faeces, which may be mixed into your faeces or appear as flecks on the surface, or you may see it in the toilet or on toilet paper - get into the habit of looking into the toilet before flushing
- persistent changes in your bowel habit for several weeks - especially going to the toilet more often or having diarrhoea
- weight loss without any obvious reason and/or loss of appetite
- tiredness or breathlessness for no apparent reason - this may be caused by the small amount of blood loss from your bowel, resulting in anaemia (when there are too few red blood cells or not enough haemoglobin in your blood)
- pain, or a lump or swelling in your abdomen (tummy)
Diagnosis of bowel cancer
Your doctor will ask about your symptoms and examine you. He or she may also ask you about your medical history. Your doctor may refer you to a doctor or surgeon who specialises in colorectal disease.
Tests for bowel cancer include the following.
These tests may include:
Screening is important for detecting bowel cancer in its early stages.
You may choose to have regular screening if you:
Tests for bowel cancer include the following.
- A colonoscopy, which is a test that allows a doctor to look inside your large bowel. The test is done using a narrow, flexible, tube-like telescopic camera called a colonoscope.
- A sigmoidoscopy, which is a procedure used to look inside your rectum and the lower part of your bowel.
- A barium enema, which involves placing a fluid containing barium (a substance which shows up on X-rays) into your bowel via your rectum. X-ray images of your abdomen then show the inside of your bowel more clearly.
These tests may include:
- an ultrasound scan of your abdomen to see if the cancer has spread
- a CT scan to show the position of the tumour
- an MRI scan to show two- and three-dimensional pictures of your bowel
- a chest X-ray to check the health of your heart and lungs
- blood tests to assess your general health
Screening is important for detecting bowel cancer in its early stages.
You may choose to have regular screening if you:
- are over 50 years old
- have a close relative who has had bowel cancer
- have FAP, HNPCC, or other diseases of the bowel lining such as ulcerative colitis or Crohn's disease
Treatment of bowel cancer
The type of treatment you have will depend on the size of the tumour, its position and whether it has spread.
Surgery
Surgery is the most common treatment for bowel cancer.
If you have surgery, the part of your large bowel that contains the cancer will be removed and the two open ends joined together. Lymph nodes (glands found throughout your body that are part of your immune system) near your bowel are often removed because they are the first place the cancer usually spreads to.
Sometimes, depending on the location and size of the cancer that is removed, the two ends of your bowel can't be rejoined. If this happens, the opening nearest the beginning of your bowel will be brought out on to the skin surface of your abdomen. A colostomy is an opening of your large bowel onto the surface of your tummy (abdomen) and an ileostomy is an opening of your small bowel onto the surface of the abdomen. The opening of the bowel is known as a stoma.
A bag is worn over the stoma, which collects your bowel movements outside your body. Most people who have surgery don't need a colostomy, but if you do, it's usually temporary.
If you have cancer in your rectum, you may need surgery to remove the part of your rectum that contains the cancer, as well as the fatty tissue and lymph nodes around your rectum. You're more likely to need a colostomy if you have cancer of the rectum than if you have cancer of the colon.
Non-surgical treatments
Chemotherapy and radiotherapy
Sometimes it's not possible to remove all the cancer by surgery, so you may need to have additional treatment with chemotherapy and/or radiotherapy.
These treatments are given to destroy any remaining cancer cells and to prevent it spreading further. Chemotherapy and radiotherapy are also sometimes used to shrink the tumour before surgery or to kill any cancer cells that are left after surgery.
Chemotherapy and radiotherapy can both have side-effects.
Monoclonal antibodies
Monoclonal antibodies (MABs) are medicines that are designed to recognise and target markers that are commonly carried by cancer cells. There are three main MAB treatments for bowel cancer:
Surgery
Surgery is the most common treatment for bowel cancer.
If you have surgery, the part of your large bowel that contains the cancer will be removed and the two open ends joined together. Lymph nodes (glands found throughout your body that are part of your immune system) near your bowel are often removed because they are the first place the cancer usually spreads to.
Sometimes, depending on the location and size of the cancer that is removed, the two ends of your bowel can't be rejoined. If this happens, the opening nearest the beginning of your bowel will be brought out on to the skin surface of your abdomen. A colostomy is an opening of your large bowel onto the surface of your tummy (abdomen) and an ileostomy is an opening of your small bowel onto the surface of the abdomen. The opening of the bowel is known as a stoma.
A bag is worn over the stoma, which collects your bowel movements outside your body. Most people who have surgery don't need a colostomy, but if you do, it's usually temporary.
If you have cancer in your rectum, you may need surgery to remove the part of your rectum that contains the cancer, as well as the fatty tissue and lymph nodes around your rectum. You're more likely to need a colostomy if you have cancer of the rectum than if you have cancer of the colon.
Non-surgical treatments
Chemotherapy and radiotherapy
Sometimes it's not possible to remove all the cancer by surgery, so you may need to have additional treatment with chemotherapy and/or radiotherapy.
These treatments are given to destroy any remaining cancer cells and to prevent it spreading further. Chemotherapy and radiotherapy are also sometimes used to shrink the tumour before surgery or to kill any cancer cells that are left after surgery.
Chemotherapy and radiotherapy can both have side-effects.
Monoclonal antibodies
Monoclonal antibodies (MABs) are medicines that are designed to recognise and target markers that are commonly carried by cancer cells. There are three main MAB treatments for bowel cancer:
- bevacizumab
- cetuximab
- panitumumab
Prevention of bowel cancer
There is evidence that taking the following steps can help to reduce your risk of getting bowel cancer.
- Try to do 150 minutes (two and a half hours) of moderate exercise over a week in bouts of 10 minutes or more. You can do this by carrying out 30 minutes on at least five days each week. Alternatively, you can do 75 minutes of vigorous intensity activity.
- Eat five or more portions of fruit and vegetables every day.
- Cut down on the amount of processed and red meat you eat.
- Maintain a healthy weight.
- Eat foods high in fibre such as wholegrain bread, cereals and pasta.
- If you smoke, quit.
Disclaimer
This information was published by Bupa Group's Health Content Team and has been reviewed by appropriate medical or clinical professionals. To the best of their knowledge the information is current and based on reputable sources of medical evidence, however Bupa (Asia) Limited makes no representation or warranty as to the completeness or accuracy of the Content.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.










