Cancer that starts in your liver is called primary liver cancer. About 1,800 people are diagnosed with liver cancer each year in Hong Kong.
Cancerous tumours can grow through your liver and spread to other areas of your body, through your bloodstream or your lymphatic system, where they may grow and form secondary tumours. Your lymphatic system is the tissues and organs, including your bone marrow, spleen, thymus and lymph nodes, that produce and store cells that fight infection and disease. This spread of cancer is called metastasis.
Tumours may also spread from other parts of your body, such as from your bowel, breast or lungs, to your liver - this is called secondary liver cancer. Secondary liver cancer is much more common than primary liver cancer.
This factsheet will concentrate on primary liver cancer.
Cancerous tumours can grow through your liver and spread to other areas of your body, through your bloodstream or your lymphatic system, where they may grow and form secondary tumours. Your lymphatic system is the tissues and organs, including your bone marrow, spleen, thymus and lymph nodes, that produce and store cells that fight infection and disease. This spread of cancer is called metastasis.
Tumours may also spread from other parts of your body, such as from your bowel, breast or lungs, to your liver - this is called secondary liver cancer. Secondary liver cancer is much more common than primary liver cancer.
This factsheet will concentrate on primary liver cancer.
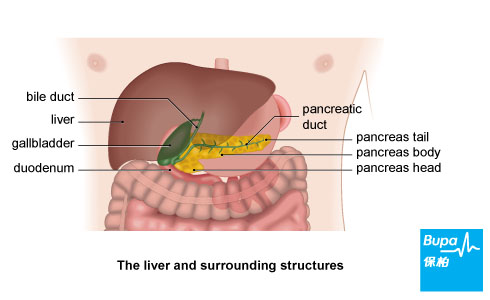
The liver
Your liver is a large organ found in the top part of your abdomen (tummy), just under your ribcage. It's split into sections called lobes.
Your liver carries out about 500 different jobs, including:
- getting rid of toxins from your body
- processing digested food
- producing bile - a digestive fluid that helps to break down fatty food
Types of primary liver cancer
There are two main types of primary liver cancer - hepatocellular carcinoma and cholangiocarcinoma. Hepatocellular carcinoma (also known as hepatoma or HCC) is the most common type of liver cancer. It starts in the main cells of your liver called hepatocytes.
Cholangiocarcinoma starts in the cells that line your bile duct and is commonly known as cancer of the bile duct. Your bile duct is a tube that connects your liver to your small bowel.
More rare types of liver cancer include:
Cholangiocarcinoma starts in the cells that line your bile duct and is commonly known as cancer of the bile duct. Your bile duct is a tube that connects your liver to your small bowel.
More rare types of liver cancer include:
- angiosarcoma - this starts in the blood vessels of your liver
- hepatoblastoma - this usually affects young children
Causes of primary liver cancer
In the UK, most people get HCC because of cirrhosis - scarring of the liver. Cirrhosis affects how well your liver is able to function. The most common cause of cirrhosis in the UK is drinking too much alcohol. It can also be caused by infections such as hepatitis B and hepatitis C. About three or four people out of every 100 with cirrhosis will develop liver cancer.
Other factors that put you more at risk of developing HCC include:
In Africa and Asia, where liver cancer is more common, a frequent cause is a substance called aflatoxin that is found in mouldy peanuts and grain. If eaten over a long period of time it can lead to liver cancer.
Doctors don't yet understand why people develop cholangiocarcinoma. However, if you have an inflammatory bowel condition such as ulcerative colitis you may be slightly more at risk.
Other factors that put you more at risk of developing HCC include:
- having haemochromatosis - a condition where your body has too much iron
- being male - liver cancer is twice as likely to occur in men as in women
- having diabetes
In Africa and Asia, where liver cancer is more common, a frequent cause is a substance called aflatoxin that is found in mouldy peanuts and grain. If eaten over a long period of time it can lead to liver cancer.
Doctors don't yet understand why people develop cholangiocarcinoma. However, if you have an inflammatory bowel condition such as ulcerative colitis you may be slightly more at risk.
Symptoms of primary liver cancer
Everyone with liver cancer will be affected differently, but it's quite likely that at first you won't have any symptoms. Later, symptoms may include:
- weight loss
- swollen abdomen
- pain and discomfort in your liver area
- feeling full or bloated after eating
- loss of appetite
- sickness
- extreme tiredness
- jaundice (a yellowy tinge to your skin and the whites of your eyes)
Diagnosis of primary liver cancer
Your doctor will ask about your symptoms and examine you. He or she may also ask about your medical history.
Your doctor may refer you to a specialist at a hospital, where you're likely to have tests including liver function tests. These tests check whether your liver is working properly by looking at a sample of your blood.
Your doctor may also check for a particular cancer marker - a protein that shows up in higher amounts if you have HCC.
Other tests you may have include the following.
Your doctor may refer you to a specialist at a hospital, where you're likely to have tests including liver function tests. These tests check whether your liver is working properly by looking at a sample of your blood.
Your doctor may also check for a particular cancer marker - a protein that shows up in higher amounts if you have HCC.
Other tests you may have include the following.
- An ultrasound scan, which uses sound waves to produce an image of your liver.
- A CT scan, which uses X-rays to make a three-dimensional picture of your liver.
- An MRI scan, which uses magnets and radiowaves to produce images of your liver.
- A biopsy, where a small sample of tissue is taken from your liver. This is sent to a laboratory for testing.
- A laparoscopy. This is a minor operation that allows a surgeon to look at your liver by inserting a thin tube containing a light and a camera through a small cut in your abdomen. Your surgeon may take a liver biopsy at the same time.
- A hepatic angiography, which is an X-ray of the blood vessels supplying your liver. This is usually done if there's doubt about your diagnosis after a CT and MRI scan.
Treatment of primary liver cancer
Treatment depends on how advanced your cancer is and on your general health. It will also vary according to exactly where the cancer is and whether it has spread to other parts of your body.
Surgery
Surgery is the only treatment that offers a cure. However, fewer than one in three people who have HCC can have surgery to remove it. This may be because the tumour is too big, the cancer has spread to other areas or your liver is too badly damaged by cirrhosis.
Surgery options include:
Non-surgical treatments
Ethanol injections
Ethanol (pure alcohol) injections can be used to treat small tumours. Ethanol is injected through your skin into the affected area during an ultrasound. It stops the blood supply to your tumour, killing the cancer cells.
Radiofrequency ablation
During an ultrasound or CT scan, a thin needle is placed in your tumour and radiowaves are passed down the needle. The radiowaves heat up the tumour and destroy it.
Chemotherapy and chemoembolisation
Chemotherapy involves using medicines to shrink the tumour and reduce your symptoms. Chemotherapy isn't very successful at treating liver cancer, but a procedure called chemoemboliation may be more effective. This means that chemotherapy medicines are mixed with an oily substance called lipiodol, which helps them to stay in your liver for longer and so have a greater effect. At the same time, tiny beads of gel are injected to block off the blood supply to your tumour.
Cryosurgery
Liquid nitrogen is placed on the tissue around the tumour to freeze and destroy the cancer.
Biological therapies
These are medicines that use substances occurring naturally in your body to kill cancer.
Surgery
Surgery is the only treatment that offers a cure. However, fewer than one in three people who have HCC can have surgery to remove it. This may be because the tumour is too big, the cancer has spread to other areas or your liver is too badly damaged by cirrhosis.
Surgery options include:
- a liver resection, where the affected part of your liver is removed (this is the most common type of surgery for liver cancer)
- a lobectomy, where a lobe of your liver is removed
- a liver transplant, where your liver is replaced with a donor's liver, however only a small number of people are suitable for this type of surgery
Non-surgical treatments
Ethanol injections
Ethanol (pure alcohol) injections can be used to treat small tumours. Ethanol is injected through your skin into the affected area during an ultrasound. It stops the blood supply to your tumour, killing the cancer cells.
Radiofrequency ablation
During an ultrasound or CT scan, a thin needle is placed in your tumour and radiowaves are passed down the needle. The radiowaves heat up the tumour and destroy it.
Chemotherapy and chemoembolisation
Chemotherapy involves using medicines to shrink the tumour and reduce your symptoms. Chemotherapy isn't very successful at treating liver cancer, but a procedure called chemoemboliation may be more effective. This means that chemotherapy medicines are mixed with an oily substance called lipiodol, which helps them to stay in your liver for longer and so have a greater effect. At the same time, tiny beads of gel are injected to block off the blood supply to your tumour.
Cryosurgery
Liquid nitrogen is placed on the tissue around the tumour to freeze and destroy the cancer.
Biological therapies
These are medicines that use substances occurring naturally in your body to kill cancer.
Disclaimer
This information was published by Bupa Group's Health Content Team and has been reviewed by appropriate medical or clinical professionals. To the best of their knowledge the information is current and based on reputable sources of medical evidence, however Bupa (Asia) Limited makes no representation or warranty as to the completeness or accuracy of the Content.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.










