In ovarian cancer, cells in your ovaries start to grow abnormally and out of control.
Ovarian cancer can sometimes spread more widely in your abdomen (tummy) or more rarely, to other organs through your bloodstream or lymphatic system. The lymphatic system is the tissues and organs, including your bone marrow, spleen, thymus, and lymph nodes, that produce and store cells that fight infection and disease. The channels that carry lymph are also part of this system. If ovarian cancer spreads to other parts of your body, it can form secondary tumours. The spread of cancer through your body is called metastasis.
Ovarian cancer can sometimes spread more widely in your abdomen (tummy) or more rarely, to other organs through your bloodstream or lymphatic system. The lymphatic system is the tissues and organs, including your bone marrow, spleen, thymus, and lymph nodes, that produce and store cells that fight infection and disease. The channels that carry lymph are also part of this system. If ovarian cancer spreads to other parts of your body, it can form secondary tumours. The spread of cancer through your body is called metastasis.
Types of ovarian cancer
There are different types of ovarian cancer. The most common is epithelial ovarian cancer, which affects the lining of the ovaries. Nine out of 10 ovarian cancers are epithelial. There are several different types of epithelial ovarian cancer; the most common type is called 'serous'.
Non-epithelial ovarian cancer is much less common. This type includes germ cell cancers that form from the cells in the ovary that make the eggs. These usually affect younger women.
Non-epithelial ovarian cancer is much less common. This type includes germ cell cancers that form from the cells in the ovary that make the eggs. These usually affect younger women.
Causes of ovarian cancer
The exact reasons why you may develop ovarian cancer aren't fully understood at present. However, there are some things that can make it more likely. It's more common in women who live in developed countries for example, and in those who have gone through the menopause. It's also known that inheriting faulty genes called BRCA1 and BRCA2 increase the risk of ovarian cancer as well as breast cancer.
Other factors that may increase your risk of getting ovarian cancer include:
Other factors that may increase your risk of getting ovarian cancer include:
- certain types of hormone replacement therapy (HRT) – especially if you take them for longer than five years
- being overweight or obese
- having endometriosis or ovarian cysts
- smoking
- starting the menopause late
- used the contraceptive pill
- had children – the more children, the lower the risk
- breastfed their children
- had a hysterectomy or been sterilised
Symptoms of ovarian cancer
Many women don't have any symptoms or only vague symptoms in the early stages of ovarian cancer. Many of these symptoms can occur in other conditions as well and are not necessarily a sign of cancer. If you do have symptoms, they may include:
- stomach pain or pain in your pelvis
- a persistent bloated feeling
- feeling full quickly and losing your appetite
- unexplained weight loss
- swelling of your abdomen
- changes in bowel or bladder habits – constipation, excess wind, diarrhoea or needing to pass urine more often
- back pain
- extreme tiredness
- rarely, abnormal vaginal bleeding
Diagnosis of ovarian cancer
Your doctor will ask you about your symptoms and examine you. He or she may also ask you about your medical history and whether anyone else in your family has had breast or ovarian cancer.
Your doctor will ask you to have a blood test to check the levels of certain proteins, such as CA125, that can be high if you have ovarian cancer. He or she may also examine you internally to check your womb and ovaries.
Your doctor may refer you to a specialist for further tests, such as an ultrasound scan or a CT scan to view the inside of your abdomen and pelvis.
If the results of your tests show you have cancer, you may need to have more tests to assess if the cancer has spread. The process of finding out the stage of a cancer is called staging.
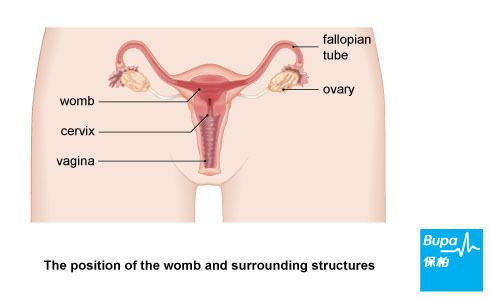
Further tests may include a gynaecological laparoscopy – this is a procedure used to examine your fallopian tubes, ovaries and womb. You may also have a small sample of tissue taken (a biopsy), which will be sent to a laboratory for testing.
If you have a build-up of fluid in your stomach, it can be drawn out through a needle and examined to see whether cancer cells are present. This is known as abdominal fluid aspiration or paracentesis.
Your doctor will ask you to have a blood test to check the levels of certain proteins, such as CA125, that can be high if you have ovarian cancer. He or she may also examine you internally to check your womb and ovaries.
Your doctor may refer you to a specialist for further tests, such as an ultrasound scan or a CT scan to view the inside of your abdomen and pelvis.
If the results of your tests show you have cancer, you may need to have more tests to assess if the cancer has spread. The process of finding out the stage of a cancer is called staging.
Further tests may include a gynaecological laparoscopy – this is a procedure used to examine your fallopian tubes, ovaries and womb. You may also have a small sample of tissue taken (a biopsy), which will be sent to a laboratory for testing.
If you have a build-up of fluid in your stomach, it can be drawn out through a needle and examined to see whether cancer cells are present. This is known as abdominal fluid aspiration or paracentesis.
Treatment of ovarian cancer
Your treatment will depend on the type of ovarian cancer you have and how far it has spread. Before you see a specialist, consider writing down any questions that you want to ask so that you don't forget them on the day.
Surgery
Almost all women with ovarian cancer will need surgery. If the cancer hasn't spread beyond your ovary, it may be possible to remove just the single affected ovary and fallopian tube.
If the cancer has already spread beyond your ovary, both ovaries and your womb, together with nearby lymph nodes and surrounding tissue, may need to be removed. This is called a total hysterectomy and oophorectomy.
Other types of surgery for more advanced ovarian cancer are used to remove, or 'debulk' as much of the tumour as possible.
Non-surgical treatments
Surgery
Almost all women with ovarian cancer will need surgery. If the cancer hasn't spread beyond your ovary, it may be possible to remove just the single affected ovary and fallopian tube.
If the cancer has already spread beyond your ovary, both ovaries and your womb, together with nearby lymph nodes and surrounding tissue, may need to be removed. This is called a total hysterectomy and oophorectomy.
Other types of surgery for more advanced ovarian cancer are used to remove, or 'debulk' as much of the tumour as possible.
Non-surgical treatments
- Chemotherapy. Chemotherapy uses medicines to destroy cancer cells. The type of chemotherapy treatment you have will vary depending on your type of ovarian cancer. Usually you have a course of treatment, which is given as several doses at intervals over a period of weeks. Your doctor will give you information on the type and course that is best for you. You will probably be offered chemotherapy after surgery to destroy any remaining cancer cells that were not removed by surgery or if there is a risk the cancer may return. However, you may have it before surgery to shrink the tumour. If ovarian cancer comes back (a relapse), you may be treated with the same chemotherapy medicine or an alternative, depending on the timing of your relapse and whether the cancer has developed resistance to previous chemotherapy medicines.
- Radiotherapy. Radiotherapy uses radiation to destroy cancer cells. It's not often used to treat ovarian cancer but is very occasionally used after surgery to destroy any remaining cancer cells. Your doctor may give you information on clinical trials that are testing new treatments for ovarian cancer. You may wish to take part in a trial as it may involve a new treatment and benefit other patients in the future.
Prevention of ovarian cancer
You may be able to reduce your risk of developing ovarian cancer by making changes to your lifestyle, such as stopping smoking and eating a healthy, balanced diet.
Getting enough vitamin D may reduce your risk of developing a number of cancers, including ovarian cancer – although more research needs to be done to be certain. Vitamin D is also well known to be important for bone health.
Vitamin D is produced naturally by your body when your skin is exposed to sunlight and can also be obtained from some foods, such as oily fish. You may get enough vitamin D during summer by spending frequent short spells in the sun without wearing sunscreen (the exact time you need is different for everyone, but is typically only a few minutes in the middle of the day).
However, do not let your skin redden. If you don't get much sun exposure and particularly during the winter months, taking up to 25 micrograms of vitamin D a day (two high-strength 12.5 microgram capsules) can help to make sure you get enough.
Always read the patient information leaflet that comes with your supplements and if you are pregnant or breastfeeding, ask your pharmacist or doctor for advice first. Talk to your doctor before taking vitamin D supplements if you are taking diuretics for high blood pressure or have a history of kidney stones or kidney failure.
Getting enough vitamin D may reduce your risk of developing a number of cancers, including ovarian cancer – although more research needs to be done to be certain. Vitamin D is also well known to be important for bone health.
Vitamin D is produced naturally by your body when your skin is exposed to sunlight and can also be obtained from some foods, such as oily fish. You may get enough vitamin D during summer by spending frequent short spells in the sun without wearing sunscreen (the exact time you need is different for everyone, but is typically only a few minutes in the middle of the day).
However, do not let your skin redden. If you don't get much sun exposure and particularly during the winter months, taking up to 25 micrograms of vitamin D a day (two high-strength 12.5 microgram capsules) can help to make sure you get enough.
Always read the patient information leaflet that comes with your supplements and if you are pregnant or breastfeeding, ask your pharmacist or doctor for advice first. Talk to your doctor before taking vitamin D supplements if you are taking diuretics for high blood pressure or have a history of kidney stones or kidney failure.
Disclaimer
This information was published by Bupa Group's Health Content Team and has been reviewed by appropriate medical or clinical professionals. To the best of their knowledge the information is current and based on reputable sources of medical evidence, however Bupa (Asia) Limited makes no representation or warranty as to the completeness or accuracy of the Content.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.










