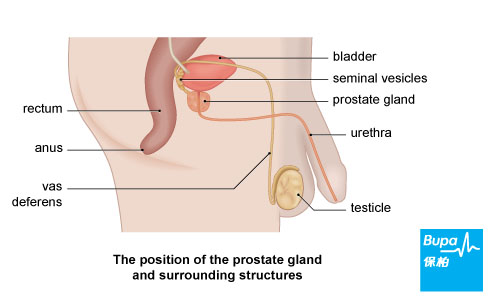
Your prostate is a gland that produces the liquid part of semen. It's about the size of a walnut and lies at the base of your bladder.
The front of your prostate surrounds your urethra - the tube that carries urine from your bladder and out through your penis. Any change in the size or shape of your prostate, such as changes that occur if you have prostate cancer, can narrow this tube, making it difficult for you to pass urine.
The front of your prostate surrounds your urethra - the tube that carries urine from your bladder and out through your penis. Any change in the size or shape of your prostate, such as changes that occur if you have prostate cancer, can narrow this tube, making it difficult for you to pass urine.
Causes of prostate cancer
The exact reasons why you may develop prostate cancer aren't fully understood at present. But you're more likely to develop prostate cancer if:
- you're over 50
- you have close relatives who have had prostate cancer
- several women in your family have had breast cancer - you may have inherited a faulty gene which may increase your risk of prostate cancer
- your diet is high in fat, meat and dairy products
Symptoms of prostate cancer
You may have:
If prostate cancer spreads to other parts of your body, other symptoms can develop such as:
- difficulty in starting to pass urine
- a weak, sometimes intermittent flow of urine
- dribbling of urine before and after urinating
- a frequent or urgent need to pass urine
- rarely, blood in your urine or semen and pain when passing urine
If prostate cancer spreads to other parts of your body, other symptoms can develop such as:
- pain in your bones, such as your back and hips
- weight loss
- impotence
Diagnosis of prostate cancer
Your doctor will ask about your symptoms and examine you. He or she may also ask you about your medical history. Your doctor may do some of the following tests, or refer you to a urologist.
- A blood test to examine the amount of prostate-specific antigen (PSA) in your blood. PSA is a protein that is made by both normal and cancerous prostate cells. The test can be inaccurate as a high PSA level doesn't always indicate cancer and can be caused by other prostate conditions.
- A digital rectal examination (DRE) - an examination of your prostate. Your doctor will feel your prostate through the wall of your rectum (back passage). If you have prostate cancer, it may feel harder than usual, or knobbly.
- A prostate biopsy, where your doctor uses a needle to remove a small piece of tissue from your prostate. The sample will be sent to a laboratory to find out if you have cancer and if so, how fast it's growing.
- An ultrasound to examine your prostate gland, using a small device inserted into your rectum.
- CT scan, MRI scan and bone scans can help your surgeon see how far the cancer has spread (if at all). Doctors are currently trialling a new urine test to look for a protein made by PCA3 (prostate cancer gene 3). However, it's not available at the moment.
Treatment of prostate cancer
Your treatment will depend on a number of factors, including your age, whether the cancer has spread, and if so, how far. There are various treatments available. Your surgeon may use treatments on their own or you may have a combination of different treatments.
Active monitoring
Sometimes, particularly for slow-growing tumours, no treatment is the best course of action. This is often called active monitoring or watchful waiting. Your condition will be closely monitored by your doctor with routine check-ups. If tests show that the cancer is growing or causing symptoms, your doctor may suggest that you start having treatment.
Surgery
Surgery is a common treatment for prostate cancer. It's most suitable for otherwise healthy men (usually, those under 70) whose cancer hasn't spread beyond their prostate. There are several types of surgery used, including:
Non-surgical treatments
Active monitoring
Sometimes, particularly for slow-growing tumours, no treatment is the best course of action. This is often called active monitoring or watchful waiting. Your condition will be closely monitored by your doctor with routine check-ups. If tests show that the cancer is growing or causing symptoms, your doctor may suggest that you start having treatment.
Surgery
Surgery is a common treatment for prostate cancer. It's most suitable for otherwise healthy men (usually, those under 70) whose cancer hasn't spread beyond their prostate. There are several types of surgery used, including:
- radical prostatectomy - a major operation to remove the whole of your prostate and some surrounding healthy tissue
- keyhole surgery (a laparoscopic prostatectomy) where your prostate is removed through smaller incisions and robot-assisted surgery
- very rarely, an orchidectomy - where your surgeon removes your testicles to get rid of the main source of the male sex hormone testosterone, which can help the cancer grow
Non-surgical treatments
- Radiotherapy, which uses X-rays to destroy cancer cells.
- Hormone therapy, which blocks the action of testosterone. This can slow the growth and spread of prostate tumours but won't kill the cancer cells. Hormone therapies include taking a medicine called bicalutamide or having injections of a medicine called goserelin.
- Chemotherapy, which uses medicines to destroy cancer cells. Your doctor may recommend a medicine called docetaxel combined with a steroid called prednisolone if hormone therapy isn't working (hormone refractory cancer).
- High intensity focused ultrasound (HIFU). This treatment uses heat to target and destroy cancer cells. It may only be available as part of a clinical trial and only if the cancer is in its early stages or if your cancer has come back.
- Cryotherapy, which uses liquid nitrogen to freeze and kill cancer cells. This may only be available as part of a clinical trial and only if your cancer is in its early stages or if your cancer has come back.
Prevention of prostate cancer
Research suggests that you may be able to reduce your risk of developing prostate cancer through certain lifestyle changes such as:
- stopping smoking
- eating a healthy, balanced diet with at least five portions of fruit and vegetables a day - especially tomatoes, which contain a substance called lycopene that may be protective
- consuming less meat and dairy products
- being physically active - you should exercise for 30 minutes at least five times a week
Disclaimer
This information was published by Bupa Group's Health Content Team and has been reviewed by appropriate medical or clinical professionals. To the best of their knowledge the information is current and based on reputable sources of medical evidence, however Bupa (Asia) Limited makes no representation or warranty as to the completeness or accuracy of the Content.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.










