The thyroid gland is an endocrine gland. It produces hormones that travel around your body in your bloodstream. Hormones are chemicals produced by the body to help control how your cells and organs work. They are sometimes called chemical messengers. The main hormones produced in your thyroid gland are thyroxine (T4) and triiodothyronine (T3). They influence the speed at which your body processes and uses energy. This is sometimes called your metabolic rate.
Hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid) are common problems associated with the levels of T3 and T4. Another hormone, called calcitonin is produced in your thyroid gland. Calcitonin works with parathyroid hormone, which is made by the parathyroid glands. Together they help to control the amount of calcium in your body, which is important for healthy bones and nerves.
Hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid) are common problems associated with the levels of T3 and T4. Another hormone, called calcitonin is produced in your thyroid gland. Calcitonin works with parathyroid hormone, which is made by the parathyroid glands. Together they help to control the amount of calcium in your body, which is important for healthy bones and nerves.
Risks of developing thyroid cancer
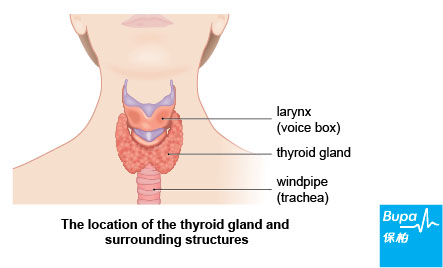
The thyroid gland is in your neck in front of your windpipe. It's quite small and flat and often difficult to see or feel. The risk of developing thyroid cancer in women is fairly constant between the age of 30 and 55, after which the risk falls. But for men, the risk of developing thyroid cancer goes up with age until 75 years. South Asian women are at a higher risk of developing thyroid cancer.
Cancerous tumours can grow through your thyroid gland and sometimes spread to other parts of your body (through your bloodstream or the lymph system) where they may grow and form secondary tumours. This spread of cancer is called metastasis. Benign tumours aren't cancerous and don't spread to other areas of the body.
Cancerous tumours can grow through your thyroid gland and sometimes spread to other parts of your body (through your bloodstream or the lymph system) where they may grow and form secondary tumours. This spread of cancer is called metastasis. Benign tumours aren't cancerous and don't spread to other areas of the body.
Types of thyroid cancer
There are four main types of thyroid cancer. These are listed below. The papillary and follicular types are sometimes grouped together and are called differentiated thyroid cancer.
- Papillary thyroid cancer is the most common type of thyroid cancer. It's usually slow growing and is most common in women and in younger people.
- ollicular thyroid cancer is less common than papillary thyroid cancer and usually affects slightly older people. It can spread to other parts of the body such as the lung or bones.
- Anaplastic thyroid cancer is also rare. It tends to grow more quickly than other types of thyroid cancer and can be more difficult to treat. About three in 20 people with thyroid cancer have this type. It's more common in older people and women.
- Medullary thyroid cancer is rare and affects about one in 20 people with thyroid cancer. For around one in every four people with medullary thyroid cancer it's a hereditary condition, which means it's passed down through family generations. It can spread to other parts of body, such as the lungs and bones.
Causes of thyroid cancer
The causes of thyroid cancer aren't fully understood at present. There are, however, certain factors that make developing thyroid cancer more likely. The following factors may increase your risk of the disease.
- History of non-cancerous (benign) thyroid disease, such as an enlarged thyroid or inflammation of the thyroid.
- Radiotherapy to the neck area, particularly if this was done at a young age.
- Not enough iodine in the diet.
- An inherited bowel condition called familial adenomatous polyposis (FAP).
- Family history of medullary thyroid cancer.
Symptoms of thyroid cancer
Lumps in the thyroid gland are quite common. For example, nine out of 10 women over the age of 70 will have a thyroid lump. If you have thyroid cancer, you may have some of the following symptoms:
These symptoms can be caused by problems other than thyroid cancer. If you have any of these symptoms, visit your doctor for advice.
- a painless lump in your neck, which gradually gets bigger
- difficulty swallowing
- breathing problems
- a hoarse voice
These symptoms can be caused by problems other than thyroid cancer. If you have any of these symptoms, visit your doctor for advice.
Diagnosis of thyroid cancer
Your doctor will ask you about your symptoms and will examine you. He or she may also ask you about your medical history and arrange initial blood tests. If your doctor thinks you may have a thyroid tumour then you will be referred to a doctor who specialises in thyroid cancer for further tests. The main tests may include the following.
- A blood sample to check, for example, the thyroid hormone levels in your blood.
- An ultrasound scan of your neck which uses sound waves to produce an image of the thyroid.
- A biopsy of a lump in your thyroid. A biopsy is a small sample of tissue. Your doctor may use an ultrasound scan to guide a needle to the thyroid lump to take a biopsy. Alternatively, a small operation may be performed under general or local anaesthesia, where a small cut is made in your neck and a biopsy is taken from the thyroid gland. This will be sent to a laboratory for testing to find out if the cells are benign (not cancerous) or cancerous.
Treatment of thyroid cancer
The treatment for thyroid cancer depends on the type, size and stage of thyroid cancer you have.
Surgery
An operation to remove all or part of the thyroid gland is the most common treatment for thyroid cancer. This is called a thyroidectomy. Lymph glands near your thyroid gland may also be removed. The type of surgery you have will depend on how far the cancer has spread.
Radioactive iodine treatment
Most people will need to have radioactive iodine treatment after surgery. This is to make sure that all the cancer cells are destroyed. Radioactive iodine is swallowed as a drink or tablet or it can be injected into your body. The thyroid cancer cells take in the radioactive iodine and this kills them, without affecting other cells in your body.
This treatment is given in hospital and you may need to stay there for a few days in a single room. This is because you will remain slightly radioactive for a few days after the treatment and should limit the time you spend with other people.
External radiotherapy
Radiotherapy is a treatment to destroy cancer cells with radiation. A beam of radiation is targeted on the cancerous cells, and shrinks the tumour. It may be the first course of treatment for anaplastic thyroid cancer, or may be used along with radioiodine in other types of thyroid cancer. Radiotherapy can also be used to treat a tumour, or part of a tumour that can't be removed with surgery. Radiotherapy is given as a course of treatment over a number of weeks.
Chemotherapy medicines
Chemotherapy uses medicines to destroy cancer cells. It's not often used to treat thyroid cancer but may be used if the cancer has spread or comes back after other treatment.
If you have had surgery to remove your thyroid gland, or if you have had some of the other treatments for thyroid cancer, you will need to take hormone replacement medicines for life. This is to replace the hormones that would have naturally been in your body if your thyroid gland was working normally.
You should have regular check-ups with your doctor to make sure you are healthy and to spot any signs of the cancer returning.
Surgery
An operation to remove all or part of the thyroid gland is the most common treatment for thyroid cancer. This is called a thyroidectomy. Lymph glands near your thyroid gland may also be removed. The type of surgery you have will depend on how far the cancer has spread.
Radioactive iodine treatment
Most people will need to have radioactive iodine treatment after surgery. This is to make sure that all the cancer cells are destroyed. Radioactive iodine is swallowed as a drink or tablet or it can be injected into your body. The thyroid cancer cells take in the radioactive iodine and this kills them, without affecting other cells in your body.
This treatment is given in hospital and you may need to stay there for a few days in a single room. This is because you will remain slightly radioactive for a few days after the treatment and should limit the time you spend with other people.
External radiotherapy
Radiotherapy is a treatment to destroy cancer cells with radiation. A beam of radiation is targeted on the cancerous cells, and shrinks the tumour. It may be the first course of treatment for anaplastic thyroid cancer, or may be used along with radioiodine in other types of thyroid cancer. Radiotherapy can also be used to treat a tumour, or part of a tumour that can't be removed with surgery. Radiotherapy is given as a course of treatment over a number of weeks.
Chemotherapy medicines
Chemotherapy uses medicines to destroy cancer cells. It's not often used to treat thyroid cancer but may be used if the cancer has spread or comes back after other treatment.
If you have had surgery to remove your thyroid gland, or if you have had some of the other treatments for thyroid cancer, you will need to take hormone replacement medicines for life. This is to replace the hormones that would have naturally been in your body if your thyroid gland was working normally.
You should have regular check-ups with your doctor to make sure you are healthy and to spot any signs of the cancer returning.
Disclaimer
This information was published by Bupa Group's Health Content Team and has been reviewed by appropriate medical or clinical professionals. To the best of their knowledge the information is current and based on reputable sources of medical evidence, however Bupa (Asia) Limited makes no representation or warranty as to the completeness or accuracy of the Content.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.










