Angina is a symptom of coronary heart disease. Based on the Population Health Survey 2003/04, 1.6% of Hong Kong people aged 15 and above had doctor-diagnosed coronary heart disease.
An episode of angina typically starts with chest pain or tightness when you are doing some sort of physical exercise. It may feel like a heavy weight or a tightening across your upper chest. Angina pain is especially likely to occur when walking after a meal. Anger or stress also tends to make it worse.
The pain may also be felt in your neck, throat or arms - making you feel that you are choking or that both arms are dead weights. The pain doesn't usually last for more than a few minutes and goes fairly quickly after resting. Indigestion and angina are often confused. As well as the pain, you may feel breathless, sweaty and have a sense of fear.
Angina affects about one in 50 people. It can often be controlled with a combination of medication and lifestyle changes.
Angina tends to happen when extra demands are placed on the heart, such as when you are exercising or doing physical activity. This is because your heart needs more oxygen at these times.
An episode of angina typically starts with chest pain or tightness when you are doing some sort of physical exercise. It may feel like a heavy weight or a tightening across your upper chest. Angina pain is especially likely to occur when walking after a meal. Anger or stress also tends to make it worse.
The pain may also be felt in your neck, throat or arms - making you feel that you are choking or that both arms are dead weights. The pain doesn't usually last for more than a few minutes and goes fairly quickly after resting. Indigestion and angina are often confused. As well as the pain, you may feel breathless, sweaty and have a sense of fear.
Angina affects about one in 50 people. It can often be controlled with a combination of medication and lifestyle changes.
Angina tends to happen when extra demands are placed on the heart, such as when you are exercising or doing physical activity. This is because your heart needs more oxygen at these times.
Types of angina
There are three main types of angina:
Stable angina
This is angina that is brought on by exertion. It happens when the blood vessels supplying your heart become narrowed, restricting the blood supply. The angina pain usually lasts for only a few minutes and goes away when you rest. But the pain may return when the effort begins again. This can usually be well controlled with medication.
Unstable angina
Unstable angina means that the pain comes on after only a little effort (such as just taking a few steps) or even when you are resting. It usually happens when one of the blood vessels supplying your heart becomes so narrowed that you are at immediate risk of a heart attack. If you get sudden chest pain like this, you should call for emergency help. If your chest pain is coming on with less and less exercise over a relatively short period of time, this is also a cause of concern and you should contact your doctor.
Variant angina
This rare type of angina occurs without warning. It is due to spasm of a coronary artery. You may need further tests to diagnose this type of angina. During an attack, there can be irregularities in your hearts normal rhythm.
Stable angina
This is angina that is brought on by exertion. It happens when the blood vessels supplying your heart become narrowed, restricting the blood supply. The angina pain usually lasts for only a few minutes and goes away when you rest. But the pain may return when the effort begins again. This can usually be well controlled with medication.
Unstable angina
Unstable angina means that the pain comes on after only a little effort (such as just taking a few steps) or even when you are resting. It usually happens when one of the blood vessels supplying your heart becomes so narrowed that you are at immediate risk of a heart attack. If you get sudden chest pain like this, you should call for emergency help. If your chest pain is coming on with less and less exercise over a relatively short period of time, this is also a cause of concern and you should contact your doctor.
Variant angina
This rare type of angina occurs without warning. It is due to spasm of a coronary artery. You may need further tests to diagnose this type of angina. During an attack, there can be irregularities in your hearts normal rhythm.
Angina and heart attack
If a coronary artery becomes completely blocked, the section of heart muscle supplied by that artery will die, unless the blockage is relieved quickly. This is a heart attack, also called a myocardial infarction or MI. The pain is more severe and prolonged than angina and isn't relieved by your usual angina treatment. If you are having a heart attack, you may also feel sick, breathless and sweaty, and may vomit. Sometimes, however, there are no symptoms at all. If you suspect that you, or someone else is having a heart attack, call for emergency help.
Causes of angina
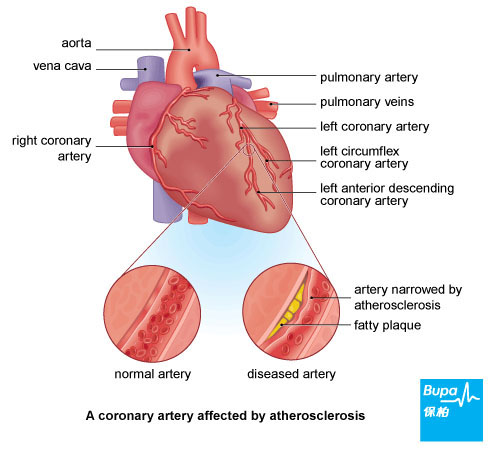
Angina is due to a narrowing of the coronary arteries - the vessels that supply the heart with blood. These arteries become furred up with fatty deposits, a process called atherosclerosis, leading to coronary heart disease.
As well as atherosclerosis, other rarer problems can also lead to angina, including:
As well as atherosclerosis, other rarer problems can also lead to angina, including:
- heart valve disease
- anaemia (a reduced amount of red blood cells in your blood)
- fast, abnormal heart rhythms
- diseases of the heart muscle
- a spasm or cramping of coronary arteries (see Variant angina)
- have a high blood cholesterol level
- have high blood pressure
- have diabetes
- smoke
- do little physical activity
Diagnosis of angina
If you have noticed a pain in your chest when you exert yourself, you should visit your doctor as soon as possible. Your doctor will ask you a number of questions about the pain and then examine you. He or she will listen to your heart and chest, check your blood pressure, and look for any signs of anaemia.
If you develop a sudden pain in your chest, you should call for emergency help.
You may need to have some further tests to help diagnose if you have a heart condition. These can include:
If you develop a sudden pain in your chest, you should call for emergency help.
You may need to have some further tests to help diagnose if you have a heart condition. These can include:
- an ECG (electrocardiogram), where your hearts electrical activity is measured, either while you are lying down or exercising on a treadmill
- blood tests, such as a blood count, cholesterol and lipid levels, and cardiac enzymes (which are released by damaged heart cells)
- an echocardiogram, where an ultrasound probe is run over your chest so that the hearts chambers and valves can be seen working
- an angiogram, where a dye visible on X-rays is injected into your coronary arteries to show up any narrowing or blockages
Treatment of angina
Any conditions you have that are causing your angina, such as high blood pressure, will be treated, as well as your angina symptoms.
Medicines
Short-term treatment of symptoms
For people with severe angina, the best treatment may be surgery or angioplasty.
Angioplasty
Angioplasty (also known as percutaneous coronary intervention or PCI). A miniature collapsed balloon is threaded through the blood vessels until it reaches the arteries of the heart. The balloon is inflated to widen the blocked coronary artery. A stent (flexible mesh tube) is sometimes inserted to help keep your artery open afterwards. Sometimes a coated stent is used as this releases a drug that helps to keep the blood vessel open.
Coronary artery bypass graft
Coronary artery bypass graft (CABG). Vessels from your legs or chest are used to bypass the blockage. This is open-heart surgery and requires a longer stay in hospital.
Medicines
Short-term treatment of symptoms
- Glyceryl trinitrate (GTN). This is a short-acting nitrate prescribed to provide relief during attacks. It comes as a spray (used in the mouth) or tablets (placed under the tongue) to take when an angina episode starts. It works by relaxing the coronary arteries so that more blood can flow through them and reach the heart muscle.
- Aspirin. If you have unstable angina, you will probably be given aspirin as soon as you are admitted to hospital, to help stop your blood from clotting and prevent a heart attack.
- Heparin. This is another medicine that prevents the blood from clotting. You will probably be given a heparin if you have unstable angina, while you are in hospital.
- Aspirin. You will probably be prescribed a small daily dose of aspirin if you have stable angina, as it lowers the risk of having a heart attack. However, aspirin increases your risk of stomach problems such as ulcers or indigestion, so its not suitable for everyone. Ask your doctor for advice about whether you should take aspirin.
- Beta-blockers (eg atenolol, bisoprolol). These slow your heart rate and the pumping power of the heart. This reduces your hearts demand for oxygen. Beta-blockers aren't suitable for people with asthma.
- Long-acting nitrates (eg isosorbide mononitrate). These widen the coronary arteries to improve blood flow to the heart. They are available as tablets or patches.
- Calcium-channel blockers (eg nifedipine). These relax the coronary arteries and other blood vessels, and reduce the force of the contraction of the heart.
- Potassium-channel activators (eg nicorandil). These relax coronary arteries to increase blood flow.
- Statins (eg simvastatin). These help reduce your cholesterol level, preventing fatty deposits in your coronary arteries from building up further.
For people with severe angina, the best treatment may be surgery or angioplasty.
Angioplasty
Angioplasty (also known as percutaneous coronary intervention or PCI). A miniature collapsed balloon is threaded through the blood vessels until it reaches the arteries of the heart. The balloon is inflated to widen the blocked coronary artery. A stent (flexible mesh tube) is sometimes inserted to help keep your artery open afterwards. Sometimes a coated stent is used as this releases a drug that helps to keep the blood vessel open.
Coronary artery bypass graft
Coronary artery bypass graft (CABG). Vessels from your legs or chest are used to bypass the blockage. This is open-heart surgery and requires a longer stay in hospital.
Prevention of angina
There are several practical steps that you can take to help prevent angina attacks and help stop your angina progressing to a heart attack.
- If you smoke, give up. Stopping smoking is difficult, so ask your doctor or pharmacist for advice.
- If you are overweight, try to lose excess weight.
- Eat a low-fat, high-fibre diet, rich in fruit and vegetables.
- Try to eat oily fish, such as sardines or salmon, once a week.
- Drink alcohol in moderation.
- Take regular exercise. Moderate aerobic exercise such as brisk walking, cycling or swimming is recommended. Get advice from your doctor or practice nurse on how much exercise you can do without any problems, and gradually increase it over time.
- Reduce stress where possible. You may find that learning relaxation techniques will help you with this.
- Attend regular check-ups with your doctor to monitor your blood pressure and get advice on how to reduce it if necessary.
- If you have diabetes, you should aim to closely control your blood sugar levels, as advised by your nurse or doctor.
- Your doctor will also monitor your cholesterol level - if it's too high, your doctor can advise you about your options for reducing it.
Disclaimer
This information was published by Bupa Group's Health Content Team and has been reviewed by appropriate medical or clinical professionals. To the best of their knowledge the information is current and based on reputable sources of medical evidence, however Bupa (Asia) Limited makes no representation or warranty as to the completeness or accuracy of the Content.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.










