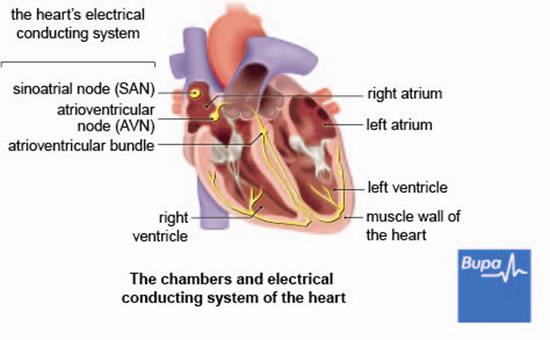
The usual pattern of a heartbeat starts when an electrical impulse is produced by part of your heart called the sinus node. The impulse is conducted to the top chambers of your heart (the left atrium and right atrium). This causes them to contract, pushing your blood into two lower, larger chambers (the left and right ventricles). The electrical impulse is then transmitted to the ventricles causing them to contract. This pushes the blood out of your heart to your lungs and the rest of your body.
Your heart will usually beat between 60 and 100 times a minute when you're resting. There are certain times when it may beat faster or slower than this, for example if you're exercising or depending on how fit you are.
Your heart will usually beat between 60 and 100 times a minute when you're resting. There are certain times when it may beat faster or slower than this, for example if you're exercising or depending on how fit you are.
Types of arrhythmia
- Sinus tachycardia. This is when your heartbeat is still regular, but faster than it should be. It's normal in certain situations, such as during exercise or if you have a fever, but may also occur at other times for no obvious reason. Conditions such as an overactive thyroid gland or anaemia may cause sinus tachycardia. Although normal heart rate can reach 100 beats per minute (bpm) when you're at rest, you may feel some discomfort if the rate is faster than you're used to for a particular level of activity.
- Sinus bradycardia. This is when your heartbeat is still regular, but slower than usual (fewer than 60 bpm). Bradycardia is common in athletes but can also occur if you're exposed to the cold and have a low body temperature or are resting or sleeping. If your heart rate is extremely slow, you may feel dizzy or faint.
- Ectopic beats. These are extra heartbeats but they don't result in any blood being pumped from your heart. You feel an ectopic heartbeat as a missed beat and the next beat is then more powerful – you feel this as a thump. You may get ectopic beats every few beats or even every beat – this results in a slow, thumping rhythm (bigeminy). Ectopic beats are very common and rarely mean that you have a heart problem. They are most noticeable when you're resting.
Atrial fibrillation
Atrial fibrillation is the most common type of arrhythmia and happens when the electrical impulses in your atria become disorganised, which overrides your heart's normal rate and rhythm. This causes your atria to contract in an irregular manner or 'fibrillate'. You may notice that your heartbeat feels uneven and it may be faster than usual. Attacks of atrial fibrillation can last from a few seconds to over a week, and can cause symptoms including:
- palpitations – an unpleasant awareness of your heartbeat, often described as a thumping in your chest
- tiredness – not being able to do as much physical activity as usual
- breathlessness
- dizziness or fainting
- chest pain
Supraventricular tachycardia
There are different types of supraventricular tachycardia (SVT) and most are caused by one or more extra electrical pathways in your heart, between the atria and the ventricles. This allows electrical impulses to 'short-circuit' and re-enter your atria instead of going to your ventricles. This means that the impulses end up travelling around your heart in a circle.
SVT can make your heart beat very quickly, possibly 250 beats per minute or more. Attacks of SVT may only last for a few seconds but can last for several hours or, rarely, days.
Ventricular tachycardia
In ventricular tachycardia, the electrical impulses fire too quickly from your ventricles, causing blood to be pumped out faster than usual. Your ventricles may not have enough time to fill up properly with blood and this can sometimes cause your heart to stop pumping blood around your body (cardiac arrest).
If the attack lasts for 30 seconds or more, it's called sustained ventricular tachycardia. Ventricular tachycardia can progress to a condition called ventricular fibrillation.
Ventricular fibrillation
In ventricular fibrillation, electrical impulses start firing from multiple sites in your ventricles, very rapidly and in an irregular rhythm. This means your heart can't beat properly and little or no blood will be pumped. Ventricular fibrillation is a type of cardiac arrest, which can be fatal. You will lose consciousness and your pulse and breathing will stop. A cardiac arrest needs urgent medical treatment – it's vital to get emergency cardiopulmonary resuscitation (CPR) straight away.
Heart block
If you have heart block, it means there is a problem affecting how the electrical impulses are transmitted from your atria to your ventricles. There are different types of heart block – it can occur in your atrioventricular (AV) node or in the muscle fibres that lead into your ventricles. Your AV node is found between the upper and lower chambers of your heart. The symptoms of heart block vary and you may or may not need treatment depending on how severe they are.
Tachy-brady syndrome
In tachy-brady syndrome (also called sick sinus syndrome), your sinus node doesn't function properly and causes your heart to beat slowly and then fast and abnormally. This can cause you to feel dizzy or collapse.
Causes of arrhythmia
An arrhythmia can be caused by a number of things. This includes certain conditions such as:
Often it may not be possible to find a cause for your arrhythmia. It's important to remember that having an arrhythmia doesn't necessarily mean that you have a serious heart problem.
- heart failure
- heart valve disease
- inflammation of your heart (myocarditis)
- thyroid disease
- diabetes
- high blood pressure
- a heart attack
- coronary heart disease
- chronic obstructive pulmonary disease (COPD)
- Wolff-Parkinson-White syndrome – an electrical abnormality in the heart that can cause SVT and atrial fibrillation
Often it may not be possible to find a cause for your arrhythmia. It's important to remember that having an arrhythmia doesn't necessarily mean that you have a serious heart problem.
Symptoms of arrhythmia
Your symptoms will depend on the type and severity of your arrhythmia. How often you get them will also vary, ranging from every day to very infrequently, once or twice a year for example. With some types of arrhythmia you may not get any symptoms, but general ones include:
- palpitations
- dizziness
- fainting or collapsing
- breathlessness
- chest pain
- tiredness
Diagnosis of arrhythmia
Your doctor will ask about your symptoms and examine you. He or she may refer you to a cardiologist (a doctor who specialises in identifying and treating conditions of the heart and blood vessels).
Your doctor may do tests including:
Your doctor may do tests including:
- blood tests
- an electrocardiogram (ECG) – this records the electrical activity of your heart to see how well it's working
- a 24-hour heart monitor (ambulatory ECG) – this records the electrical activity of your heart over 24 hours or longer
- an electrophysiological study – this determines if you have any extra electrical pathways in your heart that are causing an abnormal heart rhythm
- an echocardiogram – this uses ultrasound (sound waves) to look at your heart's structure, valves and pumping action
- an exercise ECG – this can check for other problems with your heart and may trigger abnormal heart rhythms
Treatment of arrhythmia
Your treatment will depend on the type, cause and severity of the arrhythmia that you have.
Self-help
Sometimes, such as with ectopic beats, you may not need any treatment because your arrhythmia is unlikely to cause serious problems. Try to steer clear of any triggers of your arrhythmia that you know about, such as alcohol or caffeine. Ask your doctor for advice about exercising.
Medicines
Your doctor may prescribe medicines to help control your heart rhythm. These can include medicines to slow down your heart rate, such as beta-blockers, or antiarrhythmic medicines, such as amiodarone and flecainide – these work in different ways to control your heartbeat.
If you have atrial fibrillation, you may be advised to take blood-thinning medicines, such as warfarin, to reduce your risk of blood clots forming.
Procedures
If you need to have surgery, the exact procedure you have will depend on your condition. Your doctor will advise you which one is most suitable for you.
Cardioversion
This may be carried out if you have atrial fibrillation. In this procedure, your doctor will apply a controlled electric shock to your chest from a machine called a defibrillator. This aims to help restore your heart to its usual rhythm. Cardioversion is usually done under general anaesthetic, which means you will be asleep during the procedure, but it can sometimes be done using only a sedative – this relieves anxiety and helps you to relax.
Pacemaker
Your doctor may suggest having a pacemaker if you have heart block or sinus node disease. A pacemaker is a small device, usually implanted under your skin in the upper part of your chest. Electrical signals are sent from the pacemaker to your heart to stimulate it to beat at a specific rate. Your doctor will usually fit your pacemaker under local anaesthesia – this will block pain from your chest area and you will stay awake during the operation.
Catheter ablation therapy
You may have this procedure for atrial fibrillation, supraventricular tachycardia or ventricular tachycardia. In this procedure, your doctor identifies the abnormal areas in your heart and then inserts a catheter into your heart, via a large vein in your groin. Heat or freezing treatment is used destroy the area that is causing the abnormal rhythm. The procedure is usually done under local anaesthesia.
Ablation of the AV node
If you have atrial fibrillation, it's possible that your doctor will use catheter ablation to destroy your AV node. You will probably have a pacemaker fitted before the procedure is carried out.
Implantable cardioverter defibrillator
An implantable cardioverter defibrillator (ICD) is similar to a pacemaker. If your doctor thinks you may be at risk of a ventricular arrhythmia, you may be fitted with an ICD. This can monitor your heart rhythm and deliver a small electric shock to correct your heartbeat if it detects a problem. ICDs are usually fitted under local anaesthetic in the same way as a pacemaker.
Availability and use of different treatments may vary from country to country. Ask your doctor for advice on your treatment options.
Self-help
Sometimes, such as with ectopic beats, you may not need any treatment because your arrhythmia is unlikely to cause serious problems. Try to steer clear of any triggers of your arrhythmia that you know about, such as alcohol or caffeine. Ask your doctor for advice about exercising.
Medicines
Your doctor may prescribe medicines to help control your heart rhythm. These can include medicines to slow down your heart rate, such as beta-blockers, or antiarrhythmic medicines, such as amiodarone and flecainide – these work in different ways to control your heartbeat.
If you have atrial fibrillation, you may be advised to take blood-thinning medicines, such as warfarin, to reduce your risk of blood clots forming.
Procedures
If you need to have surgery, the exact procedure you have will depend on your condition. Your doctor will advise you which one is most suitable for you.
Cardioversion
This may be carried out if you have atrial fibrillation. In this procedure, your doctor will apply a controlled electric shock to your chest from a machine called a defibrillator. This aims to help restore your heart to its usual rhythm. Cardioversion is usually done under general anaesthetic, which means you will be asleep during the procedure, but it can sometimes be done using only a sedative – this relieves anxiety and helps you to relax.
Pacemaker
Your doctor may suggest having a pacemaker if you have heart block or sinus node disease. A pacemaker is a small device, usually implanted under your skin in the upper part of your chest. Electrical signals are sent from the pacemaker to your heart to stimulate it to beat at a specific rate. Your doctor will usually fit your pacemaker under local anaesthesia – this will block pain from your chest area and you will stay awake during the operation.
Catheter ablation therapy
You may have this procedure for atrial fibrillation, supraventricular tachycardia or ventricular tachycardia. In this procedure, your doctor identifies the abnormal areas in your heart and then inserts a catheter into your heart, via a large vein in your groin. Heat or freezing treatment is used destroy the area that is causing the abnormal rhythm. The procedure is usually done under local anaesthesia.
Ablation of the AV node
If you have atrial fibrillation, it's possible that your doctor will use catheter ablation to destroy your AV node. You will probably have a pacemaker fitted before the procedure is carried out.
Implantable cardioverter defibrillator
An implantable cardioverter defibrillator (ICD) is similar to a pacemaker. If your doctor thinks you may be at risk of a ventricular arrhythmia, you may be fitted with an ICD. This can monitor your heart rhythm and deliver a small electric shock to correct your heartbeat if it detects a problem. ICDs are usually fitted under local anaesthetic in the same way as a pacemaker.
Availability and use of different treatments may vary from country to country. Ask your doctor for advice on your treatment options.
Disclaimer
This information was published by Bupa Group's Health Content Team and has been reviewed by appropriate medical or clinical professionals. To the best of their knowledge the information is current and based on reputable sources of medical evidence, however Bupa (Asia) Limited makes no representation or warranty as to the completeness or accuracy of the Content.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.










