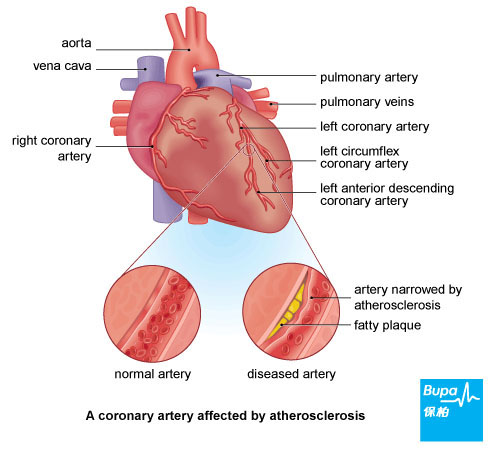
A heart attack, also known as myocardial infarction or coronary thrombosis, happens when a coronary artery (a blood vessel that supplies the heart with blood) carrying oxygen-rich blood to the heart is blocked. If the blood supply is completely blocked, part of the heart muscle may be starved of oxygen, can become damaged and may die.
Causes of a heart attack
The underlying cause of most heart attacks is atherosclerosis - this is where the coronary arteries become narrowed over many years by fatty deposits (plaques). These plaques are thought to split open (rupture), releasing substances that cause the blood flowing in the coronary artery to clot. The plaque and blood clot (thrombus) can together completely block the coronary artery, stopping blood flow to your heart and causing a heart attack.
You're more likely to have a heart attack if you:
You're more likely to have a heart attack if you:
- smoke
- have high cholesterol
- have diabetes
- have high blood pressure (hypertension)
- have a family history of heart disease
- lead an inactive lifestyle
- are overweight or obese
- drink alcohol excessively
Symptoms of a heart attack
If you have a heart attack, you will most likely feel pain or discomfort in the centre of your chest. This central chest pain is often described as a sensation of heaviness, tightness or squeezing, and may come on suddenly causing you to collapse. The pain may feel like bad indigestion.
Other symptoms may include:
During a heart attack, life-threatening heart rhythms may develop, which is why a heart attack is a medical emergency.
If you suspect that you or someone you're with is having a heart attack, call for emergency help immediately.
Other symptoms may include:
- pain spreading to the jaw, neck, arms, back or stomach
- feeling sweaty or breathless
- feeling light headed or dizzy
- feeling sick or vomiting
During a heart attack, life-threatening heart rhythms may develop, which is why a heart attack is a medical emergency.
If you suspect that you or someone you're with is having a heart attack, call for emergency help immediately.
Complications of a heart attack
Complications from a heart attack can vary widely from person to person. Some people may have few complications, whereas others may have many.
In the first few days of surviving a heart attack you may have an irregular heart beat, known as arrhythmia. You may also get angina, which is pain or discomfort in the chest after having a heart attack.
A heart attack can damage your heart muscle and cause your heart's pumping action to be weaker, making it more difficult to pump enough blood and oxygen around the body. This is known as heart failure. The larger the area of your heart muscle damaged by a heart attack, the more likely you are to have heart failure.
It's also common for people to feel low or depressed after having a heart attack. You may be worried about having another heart attack or concerned about your recovery. If you're worried about how you're feeling, speak to your GP for advice.
It's very rare but other complications may include blood clots in the lungs, rupture of the heart muscle, inflammation of the membrane covering the heart (pericarditis), or a bulging weakness in the heart muscle (aneurysm).
In the first few days of surviving a heart attack you may have an irregular heart beat, known as arrhythmia. You may also get angina, which is pain or discomfort in the chest after having a heart attack.
A heart attack can damage your heart muscle and cause your heart's pumping action to be weaker, making it more difficult to pump enough blood and oxygen around the body. This is known as heart failure. The larger the area of your heart muscle damaged by a heart attack, the more likely you are to have heart failure.
It's also common for people to feel low or depressed after having a heart attack. You may be worried about having another heart attack or concerned about your recovery. If you're worried about how you're feeling, speak to your GP for advice.
It's very rare but other complications may include blood clots in the lungs, rupture of the heart muscle, inflammation of the membrane covering the heart (pericarditis), or a bulging weakness in the heart muscle (aneurysm).
Diagnosis of a heart attack
When you get to hospital, a doctor or nurse will ask you about your symptoms and examine you. He or she will also ask you about your medical history. You may have:
- a physical examination – this involves measuring your blood pressure and monitoring your heart rate
- blood tests to check for any damage to your heart muscle
- an ECG – this checks the electrical activity of your heart and helps to diagnose any partial or complete blockages of your coronary arteries
- a coronary angiogram – a test that uses an injection of a special dye into the blood vessels to make them clearly visible on X-ray images
- an echocardiogram – this uses ultrasound (sound waves) to show the pumping action of your heart and valves
Treatment of a heart attack
Emergency medical treatment is vital – getting to hospital quickly and receiving specialist care greatly improves your chance of survival. If you have some aspirin, chew a single tablet, unless you know that you're allergic to it. Aspirin reduces blood clots and can help to prevent the clot that is blocking the artery from spreading.
In response to an emergency call for a suspected heart attack, the ambulance service will send a paramedic as soon as possible. Sit and rest in a position that is most comfortable until the paramedics arrive. He or she will give you initial treatment and provide transport to a hospital quickly and safely for further treatment. You may also be given oxygen and medicines for pain relief.
During or after a heart attack, you may have an irregular heart beat, known as arrhythmia. The most serious form of this is called ventricular fibrillation. This is when the electrical activity of the heart becomes chaotic and the heart stops pumping, and quivers or ‘fibrillates’ instead. This is known as a cardiac arrest and the paramedic may need to use a defibrillator, which gives a large electric shock through the wall of your chest and can restore a regular heartbeat.
Hospital treatment
Your treatment will depend on how severe your heart attack was. Once you arrive at hospital, your doctor will decide on the best treatment for you.
There are two commonly used ways to restore blood flow in a blocked artery.
After treatment of a heart attack
After a heart attack, you may need to take medicines regularly for a long time. Medicines you may be prescribed include aspirin, antiplatelets (eg clopidogrel or prasugrel), statins (eg simvastatin), angiotensin-converting enzyme (ACE) inhibitors (eg ramipril), and beta-blockers (eg propranolol). A fish oil capsule (Omacor) may also be given.
Your risk of further heart attacks can be reduced by taking these medicines. Always read the patient information leaflet that comes with your medicine.
For the best possible recovery after a heart attack, you can start a cardiac rehabilitation programme. These usually include an exercise regime devised by a physiotherapist (a health professional who specialises in maintaining and improving movement and mobility), along with advice on relaxation, lifestyle and treatment choices. A cardiac rehabilitation programme usually lasts between 11 and 16 sessions and ideally begins when you're admitted to hospital and continues after you leave.
In response to an emergency call for a suspected heart attack, the ambulance service will send a paramedic as soon as possible. Sit and rest in a position that is most comfortable until the paramedics arrive. He or she will give you initial treatment and provide transport to a hospital quickly and safely for further treatment. You may also be given oxygen and medicines for pain relief.
During or after a heart attack, you may have an irregular heart beat, known as arrhythmia. The most serious form of this is called ventricular fibrillation. This is when the electrical activity of the heart becomes chaotic and the heart stops pumping, and quivers or ‘fibrillates’ instead. This is known as a cardiac arrest and the paramedic may need to use a defibrillator, which gives a large electric shock through the wall of your chest and can restore a regular heartbeat.
Hospital treatment
Your treatment will depend on how severe your heart attack was. Once you arrive at hospital, your doctor will decide on the best treatment for you.
There are two commonly used ways to restore blood flow in a blocked artery.
- Thrombolysis. This is an injection to break down the clot in your coronary artery. Your chance of making a full recovery from your heart attack is much better if the clot is dissolved. However, thrombolytic medicines can increase your risk of bleeding and having a stroke so you may not be given these if you're at an increased risk of this, for example if you have recently had surgery.
- A coronary angioplasty. This can be done as an emergency procedure (also known as a primary angioplasty) or as a planned procedure. A coronary angioplasty aims to widen your artery by inflating a balloon in your narrowed or blocked coronary artery. A wire mesh tube called a stent is usually inserted to hold the coronary artery open.
After treatment of a heart attack
After a heart attack, you may need to take medicines regularly for a long time. Medicines you may be prescribed include aspirin, antiplatelets (eg clopidogrel or prasugrel), statins (eg simvastatin), angiotensin-converting enzyme (ACE) inhibitors (eg ramipril), and beta-blockers (eg propranolol). A fish oil capsule (Omacor) may also be given.
Your risk of further heart attacks can be reduced by taking these medicines. Always read the patient information leaflet that comes with your medicine.
For the best possible recovery after a heart attack, you can start a cardiac rehabilitation programme. These usually include an exercise regime devised by a physiotherapist (a health professional who specialises in maintaining and improving movement and mobility), along with advice on relaxation, lifestyle and treatment choices. A cardiac rehabilitation programme usually lasts between 11 and 16 sessions and ideally begins when you're admitted to hospital and continues after you leave.
Prevention of a heart attack
You can reduce your risk of having a heart attack by adopting a healthy lifestyle. This includes:
- not smoking
- losing excess weight
- doing regular physical activity, for 30 minutes at least five days a week
- eating a low-fat and high-fibre diet with five portions of fruit and vegetables a day and two portions of fish (one oily) a week
- not drinking more than four units of alcohol a day for men or three units a day for women
Disclaimer
This information was published by Bupa Group's Health Content Team and has been reviewed by appropriate medical or clinical professionals. To the best of their knowledge the information is current and based on reputable sources of medical evidence, however Bupa (Asia) Limited makes no representation or warranty as to the completeness or accuracy of the Content.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites. Last updated August 2017.










