A colposcopy is an examination that uses a special instrument called a colposcope to look at any ‘abnormal’ or precancerous cells which you may have in the neck of your womb (cervix).
You’ll meet the doctor or specialist nurse carrying out your examination to discuss your care. It may differ from what’s described here as it’ll be designed to meet your individual needs.
You’ll meet the doctor or specialist nurse carrying out your examination to discuss your care. It may differ from what’s described here as it’ll be designed to meet your individual needs.
When would I need to have a colposcopy?
If you’re a woman including and between the ages of 25 and 64, you’ll be offered cervical screening to check for any ‘abnormal’ or precancerous cells in your cervix. These cells aren’t cancerous, but in some women can develop into cancer later on. If you have abnormal cells, you may need to have a colposcopy so that your doctor or specialist nurse can look at your cervix in more detail.
More information
If you have cells that are thought to have either borderline (very slight) changes or be ‘low grade’ (i.e. they show mild changes), the cells will be tested for the human papillomavirus (HPV). They’ll be tested because HPV is known to cause cervical cancer. If you have the virus, you’ll need to have a colposcopy – if not, you won’t and can go back to routine screening.
If you have abnormal cells that are thought to be high grade (with either moderate or severe changes), you’ll have a colposcopy without being tested for HPV first.
It’s rare, but your doctor or nurse may notice that your cervix looks abnormal during screening. If this happens, you’ll need to have a colposcopy to investigate this.
If you have symptoms that could mean you have cervical cancer, your GP will refer you to a gynaecologist (a doctor who specialises in women’s reproductive health). Depending on what they find, you may be referred for a colposcopy. Symptoms that could mean you have cervical cancer include:
More information
If you have cells that are thought to have either borderline (very slight) changes or be ‘low grade’ (i.e. they show mild changes), the cells will be tested for the human papillomavirus (HPV). They’ll be tested because HPV is known to cause cervical cancer. If you have the virus, you’ll need to have a colposcopy – if not, you won’t and can go back to routine screening.
If you have abnormal cells that are thought to be high grade (with either moderate or severe changes), you’ll have a colposcopy without being tested for HPV first.
It’s rare, but your doctor or nurse may notice that your cervix looks abnormal during screening. If this happens, you’ll need to have a colposcopy to investigate this.
If you have symptoms that could mean you have cervical cancer, your GP will refer you to a gynaecologist (a doctor who specialises in women’s reproductive health). Depending on what they find, you may be referred for a colposcopy. Symptoms that could mean you have cervical cancer include:
- bleeding in between your periods, or after sex
- vaginal discharge that is stained with blood
- pain in your pelvis
What are the alternatives to colposcopy?
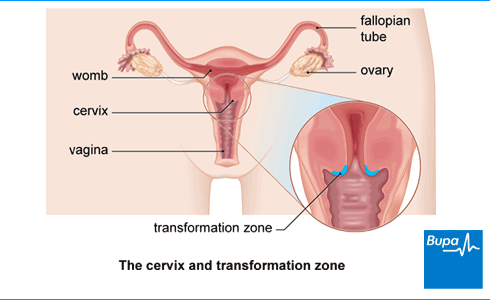
If the abnormal cells on your cervix can´t be seen properly with a colposcope, you may need to have a cone biopsy or LLETZ (large loop excision of the transformation zone) to remove the abnormal cells.
What happens before the procedure?
Before a colposcopy, your colposcopist (a doctor or specialist nurse, trained in colposcopy) will explain your cervical cytology, or ‘smear’, results to you. They’ll also discuss your general health and wellbeing and explain the examination to you. You’ll need to give your consent for the colposcopy to go ahead, so it's important that you understand what’s involved and ask any question you may have before the examination.
Some doctors prefer not to carry out a colposcopy if you have your period. Try to arrange your appointment for a date when you won’t have your period.
If you are pregnant, or think you might be, let your doctor know as the colposcopy may need to be done in a slightly different way.
Some doctors prefer not to carry out a colposcopy if you have your period. Try to arrange your appointment for a date when you won’t have your period.
If you are pregnant, or think you might be, let your doctor know as the colposcopy may need to be done in a slightly different way.
What happens during a colposcopy?
A colposcopy usually takes between 15 and 30 minutes.
You will be required to remove all clothing from the bottom half of your body. Your colposcopist (a doctor or specialist nurse, trained in colposcopy) will ask you to lie on your back on a special couch, with your feet drawn up, and your knees apart and bent. There may be leg or pedal rests to support your legs or feet.
Your colposcopist will use a piece of equipment called a speculum (the same instrument that is used during a cervical smear test) to hold open your vagina. They’ll then put special solutions on the surface of your cervix to show up any abnormal cells more clearly.
Your colposcopist uses a colposcope (a special magnifying instrument that has a light attached to it) to look at the cells on your cervix. The colposcope will stay outside of your body the whole time.
During the examination, your colposcopist may take a biopsy (small piece of tissue) from your cervix to send to the laboratory for testing. They may put a special liquid on to the biopsied area, which acts like a bandage. The biopsy may be uncomfortable, but will only last for a few seconds. If you’re concerned, talk to your colposcopist about this.
From your biopsy, your doctor will learn if you have any precancerous cell changes, or cervical cancer.
You will be required to remove all clothing from the bottom half of your body. Your colposcopist (a doctor or specialist nurse, trained in colposcopy) will ask you to lie on your back on a special couch, with your feet drawn up, and your knees apart and bent. There may be leg or pedal rests to support your legs or feet.
Your colposcopist will use a piece of equipment called a speculum (the same instrument that is used during a cervical smear test) to hold open your vagina. They’ll then put special solutions on the surface of your cervix to show up any abnormal cells more clearly.
Your colposcopist uses a colposcope (a special magnifying instrument that has a light attached to it) to look at the cells on your cervix. The colposcope will stay outside of your body the whole time.
During the examination, your colposcopist may take a biopsy (small piece of tissue) from your cervix to send to the laboratory for testing. They may put a special liquid on to the biopsied area, which acts like a bandage. The biopsy may be uncomfortable, but will only last for a few seconds. If you’re concerned, talk to your colposcopist about this.
From your biopsy, your doctor will learn if you have any precancerous cell changes, or cervical cancer.
Will I need treatment after my colposcopy?
If you have abnormal or precancerous cells, your doctor may offer you treatment to remove them. This will depend on how abnormal your cells are and how far down into your cervix they go. If you need treatment, your doctor will be able to advise which option is best for you.
LLETZ (large loop excision of the transformation zone), is the most common treatment used in the UK. LLETZ uses a loop with an electric current that passes through it, to remove the abnormal cells from your cervix. Other treatments include:
A cone biopsy is a procedure to remove a cone-shaped wedge from the neck of your womb (cervix). Cone biopsies aren’t that common anymore. But if you have early cervical cancer, you may have a cone biopsy to treat it. You may also have a cone biopsy to remove abnormal cells that cannot be seen or sampled during colposcopy – this is because they go too far up into your cervix.
Unlike the other treatments, cone biopsy is done under general rather than local anaesthetic. If you have a cone biopsy, you may have period-like pains for around 24–48 hours after the procedure.
LLETZ (large loop excision of the transformation zone), is the most common treatment used in the UK. LLETZ uses a loop with an electric current that passes through it, to remove the abnormal cells from your cervix. Other treatments include:
- Cryotherapy – this is where abnormal cells are frozen and destroyed
- Laser treatment – this involves using a laser to cut out abnormal cells or destroy them
- Cold coagulation – a piece of surgical equipment that creates heat, is used to destroy any abnormal cells
A cone biopsy is a procedure to remove a cone-shaped wedge from the neck of your womb (cervix). Cone biopsies aren’t that common anymore. But if you have early cervical cancer, you may have a cone biopsy to treat it. You may also have a cone biopsy to remove abnormal cells that cannot be seen or sampled during colposcopy – this is because they go too far up into your cervix.
Unlike the other treatments, cone biopsy is done under general rather than local anaesthetic. If you have a cone biopsy, you may have period-like pains for around 24–48 hours after the procedure.
Will I be treated during my colposcopy appointment?
If you need treatment, it’s possible that your doctor will remove any abnormal cells during your colposcopy appointment. This is called a ‘see-and-treat’ appointment. The clinic should tell you about this option before you come in for your appointment. It’s your decision to go ahead with a ‘see-and-treat’ appointment. Talk to your doctor if you’re unsure about anything.
If you need treatment and don’t have a ‘see-and-treat’ appointment, your doctor will arrange for you to have any abnormal cells removed at a second appointment.
If you need treatment and don’t have a ‘see-and-treat’ appointment, your doctor will arrange for you to have any abnormal cells removed at a second appointment.
Are there any side effects?
Side-effects are the unwanted but temporary effects you may get after having an examination or procedure.
If your doctor or specialist nurse takes a biopsy during your colposcopy, you may have some mild bleeding from your vagina afterwards. You may also have a brown or black discharge from your vagina, which looks like coffee grounds, if your doctor uses a special liquid-type bandage to seal the biopsy area. These side-effects usually only last for a few days, but you may need to wear a sanitary towel during this time.
If your doctor or specialist nurse takes a biopsy during your colposcopy, you may have some mild bleeding from your vagina afterwards. You may also have a brown or black discharge from your vagina, which looks like coffee grounds, if your doctor uses a special liquid-type bandage to seal the biopsy area. These side-effects usually only last for a few days, but you may need to wear a sanitary towel during this time.
Could there be complications?
Complications are problems that occur during or after an examination or procedure. They rarely happen at colposcopy, but contact your colposcopy clinic for advice if you have any of the following symptoms:
- pain in your lower abdomen (tummy)
- heavy bleeding, or bleeding for more than seven days from your vagina
- vaginal discharge that smells foul
- a fever (high temperature)
What happens after a colposcopy?
You should feel fine straight after your procedure and can go home when you feel ready.
If you’ve had a biopsy and there’s some light bleeding, don’t have sex, use tampons or medication for your vagina until your bleeding has stopped. If you’ve had treatment, you should also avoid swimming for a couple of weeks. You should be able to drive and can go back to doing light exercise and other daily activities as normal.
You should find out about your results between four and eight weeks after your procedure.
Your doctor may tell you what grade of CIN you have. In many cases of CIN 1, cells return to normal on their own. If you have CIN 2 or CIN 3, there is more risk of cervical cancer developing. You won´t be diagnosed with cancer unless the abnormal cells break through the lining of your cervix into the tissue beneath.
You may need treatment to remove any abnormal cells. Cervical cancer can be prevented if the abnormal cells or the affected area of your cervix are removed. Your doctor will let you know whether you need treatment and what it will involve.
If you’ve had a biopsy and there’s some light bleeding, don’t have sex, use tampons or medication for your vagina until your bleeding has stopped. If you’ve had treatment, you should also avoid swimming for a couple of weeks. You should be able to drive and can go back to doing light exercise and other daily activities as normal.
You should find out about your results between four and eight weeks after your procedure.
Your doctor may tell you what grade of CIN you have. In many cases of CIN 1, cells return to normal on their own. If you have CIN 2 or CIN 3, there is more risk of cervical cancer developing. You won´t be diagnosed with cancer unless the abnormal cells break through the lining of your cervix into the tissue beneath.
You may need treatment to remove any abnormal cells. Cervical cancer can be prevented if the abnormal cells or the affected area of your cervix are removed. Your doctor will let you know whether you need treatment and what it will involve.
Common questions
1. Can I have a colposcopy if I'm pregnant?
Yes, it's safe for you to have a colposcopy if you're pregnant. Having a colposcopy while you're pregnant is safe for both you and your unborn baby. If any biopsies need to be taken, your doctor will be very careful. If you need treatment for any abnormal cells that are found during the colposcopy, this can usually wait until after your baby has been born.
2. Will having a colposcopy affect my periods?
Some women find that there are some changes in their cycle after having a colposcopy. This should settle down by itself with time and having a colposcopy shouldn't affect your periods in the long term
Some women have a heavier and sometimes more painful period than usual after having a colposcopy. Others find that their cycle has been interrupted and their periods begin earlier or later than they would normally. There is no medical reason for this as having a colposcopy shouldn't affect your uterus (womb).
You may have some blood-stained vaginal discharge after the procedure. The discharge shouldn't be any heavier than a normal period and should get progressively lighter with time. The discharge usually clears up within two weeks after the procedure, but it can sometimes last for up to six weeks.
3. Will just one biopsy be taken from my cervix or might I need to have more?
Your doctor may need to take more than one biopsy, depending on how large the area of abnormal cells is.
A biopsy is a sample of tissue which is taken from your cervix and sent to a laboratory to be examined. Your doctor will remove a small piece of tissue using a special instrument. Sometimes more than one biopsy needs to be taken. The number of biopsies you need usually depends on how large the area of abnormal cells is. Sometimes having a biopsy can be uncomfortable, but you shouldn't feel any pain.
Yes, it's safe for you to have a colposcopy if you're pregnant. Having a colposcopy while you're pregnant is safe for both you and your unborn baby. If any biopsies need to be taken, your doctor will be very careful. If you need treatment for any abnormal cells that are found during the colposcopy, this can usually wait until after your baby has been born.
2. Will having a colposcopy affect my periods?
Some women find that there are some changes in their cycle after having a colposcopy. This should settle down by itself with time and having a colposcopy shouldn't affect your periods in the long term
Some women have a heavier and sometimes more painful period than usual after having a colposcopy. Others find that their cycle has been interrupted and their periods begin earlier or later than they would normally. There is no medical reason for this as having a colposcopy shouldn't affect your uterus (womb).
You may have some blood-stained vaginal discharge after the procedure. The discharge shouldn't be any heavier than a normal period and should get progressively lighter with time. The discharge usually clears up within two weeks after the procedure, but it can sometimes last for up to six weeks.
3. Will just one biopsy be taken from my cervix or might I need to have more?
Your doctor may need to take more than one biopsy, depending on how large the area of abnormal cells is.
A biopsy is a sample of tissue which is taken from your cervix and sent to a laboratory to be examined. Your doctor will remove a small piece of tissue using a special instrument. Sometimes more than one biopsy needs to be taken. The number of biopsies you need usually depends on how large the area of abnormal cells is. Sometimes having a biopsy can be uncomfortable, but you shouldn't feel any pain.
Disclaimer
This information was published by Bupa Group's Health Content Team and has been reviewed by appropriate medical or clinical professionals. To the best of their knowledge the information is current and based on reputable sources of medical evidence, however Bupa (Asia) Limited makes no representation or warranty as to the completeness or accuracy of the Content.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites.
The information on this page, and any information on third party websites referred to on this page, is provided as a guide only. It should not be relied upon as a substitute for professional medical advice, nor is it intended to be used for medical diagnosis or treatment. Bupa (Asia) Limited is not liable for any loss or damage you suffer arising out of the use of, or reliance on, the information.
Third party websites are not owned or controlled by Bupa and any individual may be able to access and post messages on them. Bupa is not responsible for the content or availability of these third party websites.










